Too many Australians aren’t getting a flu vaccine. Why, and what can we do about it?
Australia’s childhood immunisation program gets very good uptake every year – have had all their routine vaccinations. But our influenza vaccine coverage doesn’t get such a good report card.
Looking back over , for kids aged six months to five years, we saw a peak in flu vaccine coverage at the beginning of the COVID pandemic at 46%, which then declined to 30% by the 2023 season.
While we’re still relatively early in the 2024 flu season, only under five have received their flu shot this year so far.
Although young children are a particular concern, flu vaccination rates appear to be lagging for the population as a whole. Reports indicate that , 16% fewer people were vaccinated against the flu compared with the same period last year.
So what’s going on, and what can we do to boost uptake?
Why do we vaccinate kids against the flu?
Last year, were highest in children aged five to nine, followed by those aged zero to four. This is not a new trend – we record a high number of flu cases and hospital admissions in kids every year. So far children aged zero to four have had the highest number of infections, marginally ahead of five- to nine-year-olds.
While kids are more likely to catch and spread the flu, they’re also of getting very sick from it. This particularly applies to children under five, and the flu vaccine is available for free for this age group.
The flu vaccine isn’t perfect – it may not prevent infections entirely – but it’s definitely our best chance of protection. Research has shown influenza-related visits to the GP were in vaccinated children compared with unvaccinated children.
So why are kids not receiving the vaccine?
Often, it comes down to misunderstandings about who is eligible for the vaccine or whom it’s recommended for. But we can address this issue by nudging people via .
Some parents about the vaccine, including the old dogma that it can cause the flu. The flu vaccine because it doesn’t contain live virus. Unfortunately, that myth is really sticky.
For , the challenge can be forgetting to book or accessing an appointment.
It’s not just kids at higher risk
Adults aged 65 and over are also to the flu, and can receive a . For this group, we usually get around . So far this year, of over-65s have received their flu vaccine.
Aboriginal and Torres Strait Islander people are likewise eligible for a free flu vaccine. While previously coverage rates were higher among Aboriginal and Torres Strait Islander peoples compared to the overall population, this gap has narrowed. There’s even some movement backwards, especially .
The flu vaccine is also free for pregnant women and anyone who has such as heart disease, chronic lung disease, diabetes or kidney disease.
Past studies have found flu vaccine coverage varies around the country from 39% to 76% (meaning in some jurisdictions up to 60% of pregnant women are not getting vaccinated). When it comes to adults with chronic health conditions, we don’t have a good sense of how many people receive the vaccine.
The reasons adults don’t always get the flu vaccine overlap with the reasons for children. Often are cited as the reason for not getting vaccinated, followed by time constraints.
We also know can be difficult for some people, such as those living in rural areas or experiencing financial hardship.
Filling the gaps
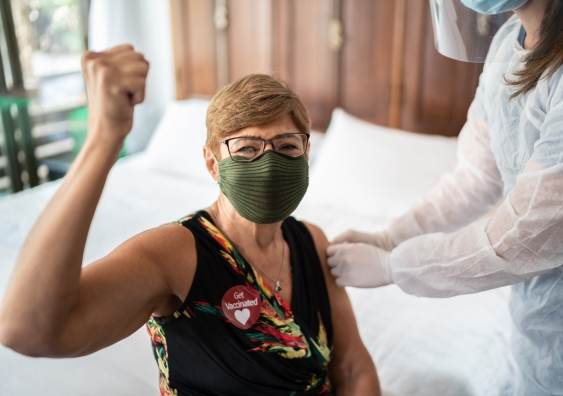
In Australia, GPs offer flu vaccines for all ages, while flu vaccination is also available at pharmacies, generally from age five and up.
While some people make a conscious decision not to get themselves or their children vaccinated, for many people, the barriers are related to access.
Programs offering vaccination outside the doctor’s office are increasing globally, and may assist in , especially among those who don’t have regular access to a GP.
For some people, their only point of contact with the may be during emergency department visits. Others may have more regular contact with a who coordinates their medical care, rather than a GP.
Offering vaccine education and programs has been shown to improve immunisation rates and may play a pivotal role in filling access gaps.
Outside medical and pharmacy settings, the workplace is the most common place for Australian adults to receive their flu vaccine. A showed Australian adults find workplace vaccination convenient and cost-effective, especially where free or subsidised vaccines are offered.
Expanding vaccination settings, such as with and mobile clinics, can benefit groups who have unique access barriers or are under-served. Meanwhile, offering vaccination through faith-based organisations has been shown to improve uptake among .
Eleftheria Lentakis, a masters student at the School of Population Health at UNSW Sydney, contributed to this article.
, Associate Professor, School of Population Health,
This article is republished from under a Creative Commons license. Read the .