Rare variants of an inflammation 'brake' gene may help reveal outcomes of kidney disease
A gene that controls inflammation could pave the way for more precise disease diagnostics and personalised treatments for kidney disease.Ìı
A gene that controls inflammation could pave the way for more precise disease diagnostics and personalised treatments for kidney disease.Ìı
Lilly Matson
UNSW Science
0426 656 007
l.matson@unsw.edu.au
The discovery of variants of an inflammation âbrakeâ gene brings scientists a step closer to personalised treatment for people at risk of kidney disease and kidney failure.Ìı
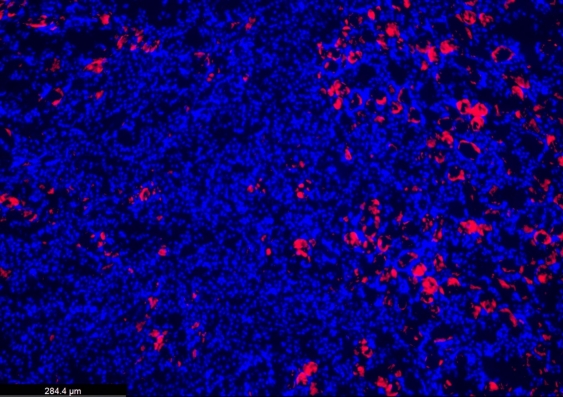
Researchers at UNSW Sydney, the , and Westmead Hospital, found that common genetic variants of TNFAIP3, which increase inflammation in the body, can paradoxically protect the kidneys from damage in the short term.ÌıÌı
âWe wanted to investigate whether inherited differences in how people regulate inflammation could lead to better or worse kidney health outcomes,â says Professor Shane Grey, senior author of the paper and Head of the School of Biotechnology and Biological Sciences (BABS) at UNSW.Ìı
The findings, published todayÌıin the journal , could be used to help determine how well people will recover from kidney injury.ÌıÌı
âOur discovery that some genetic variants can be protective against inflammation could lead to a simple genetic test that helps predict the risk of kidney disease for patients,â says Prof. Grey.Ìı Ìı
Acute kidney injury is a sudden and rapid decline in kidney function that is in part caused by inflammation. Acute kidney injury acts as an important risk factor for progression to chronic kidney disease, a major health problem affecting approximately one in 10 Australians.ÌıÌı
However, there are limited treatment options for acute kidney injury to date, and imprecise tools to predict who is most at risk of poor recovery or potential kidney failure.Ìı
Read more:ÌıÌı
The team focused their research on the TNFAIP3 gene, which produces a protein called A20, which halts the process of inflammation.ÌıÌı
âCommon variants of TNFAIP3 have been linked to autoimmune disease, but their role in kidney disease was unknown,â says Prof. Grey, who also heads the Transplant Immunology Lab at Garvan.ÌıÌı
Prof. Grey and his team started by exploring how different TNFAIP3 variants influence A20's function, finding a series of rare variants that reduced its anti-inflammatory effect. They then tested the impact of one of these variants on kidney injury in a mouse model.ÌıÌı
These tests produced unexpected results that could be used as important clues in predicting kidney disease outcomes.ÌıÌı
âDespite increasing inflammation, this rare variant surprisingly protected the kidneys from injury,â says Professor Natasha Rogers, Head of Transplantation at Westmead Hospital, who co-led the study. âWe found this protection to be due to another of A20âs functions: preventing cells from self-destructing.ÌıÌı
âOur study indicates that these âhotâ TNFAIP3 variants can alter the outcome of kidney injury, and they do so through complex effects on inflammation and cell survival,â says Prof. Rogers.Ìı Ìı

Shane Grey (left) and Natasha Rogers (right) have been researching how different variants of the TNFAIP3 gene influence inflammation. Photo: Garvan.
âMore work is needed, but these findings bring us closer to being able to predict who is at risk of poor kidney recovery, and open personalised treatment approaches,â says Professor Grey.ÌıÌı
Read more:Ìı
Down the line, the results of this study could lead to a simple genetic test to allow doctors to determine whether an individual carries a âhotâ version of the inflammation control gene, giving families greater certainty about their risk factors.Ìı
âBy gaining a better understanding of how variants of the TNFAIP3 gene influence kidney health, this research brings us closer to precision diagnostics and tailored treatments for acute kidney injury,â says Professor Grey.ÌıÌı
âRather than a one-size-fits-all approach, we may be able to determine the best way to monitor a patientâs condition based on their variant of TNFAIP3, and personalise interventions to boost their kidney recovery and long-term health.âÌı