Microbiomania: what we actually know about the human microbiome
Research into our faecal matter could lead to profound changes in the way we treat and diagnose disease. For now, though, it pays to beware of the hype.
Research into our faecal matter could lead to profound changes in the way we treat and diagnose disease. For now, though, it pays to beware of the hype.
Lance Armstrong may not have tried it, but poo doping is the new item of discussion on the performance enhancement menu.
It turns out elite cyclists have a couple of critters in their gut that might boost performance.
The discovery began three years ago, when Lauren Petersen, a researcher at The Jackson Laboratory for Genomic Medicine, in Connecticut, gave herself a poo transplant. She wiped out many of her own gut microbes with antibiotics and introduced into her bowel a tiny amount of faecal matter from a competitive cyclist.
She was trying to treat the Lyme's disease she'd had since the age of 11. Petersen happened to be a keen mountain biker and a few months later she was able to increase her training and began winning races.
The experience led her to study elite cyclists' faeces, which showed they were more likely to have a rare micro-organism called Prevotella, which helps with muscle recovery, and M. smithii, which helps turn food into energy more efficiently. Her transplant sample contained both those microbes.
When she published her work last year, the potential of poo doping became big news, although some noted that science doesn't always smell as good as it looks.
Faecal transplantation is in its infancy. While we don't quite know what is being transplanted, we do know the outcomes are not always desirable. Last year, the Royal Australasian College of Physicians Congress in Melbourne was told there was evidence to suggest transplants could cause some patients to take on the physical and mental traits of their donors, such as body shape and depression.
The interest in poo transplants is just one aspect of the intense international scientific investigation into our gut biome, the collection of micro-organisms that live in our digestive system, with new studies about it being released every few days.
“The biome is like another organ,” says Professor Emad El-Omar, Australia's leading biome specialist. “It is as heavy as the brain and as metabolically active as the liver.
“It is the interface between our genetics and our environment – the link we have long been looking for.”
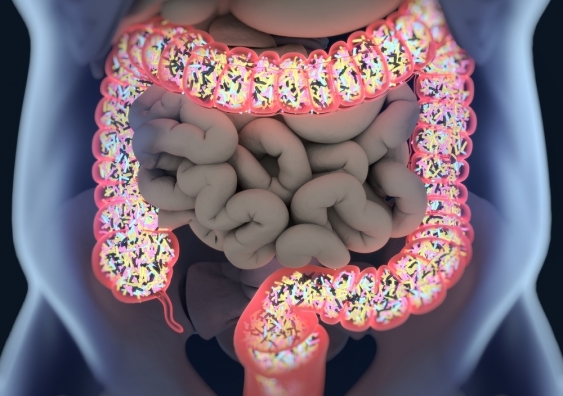
Poo is a perfect proxy for the state of the colon where a large, busy community of micro-organisms, such as bacteria, viruses and fungi, resides. These tiny tenants of the bowel are constantly interacting with each other and with their host. Together with their genes and their byproducts, they form what is now popularly called the gut biome.
Each person's biome is as unique as their fingerprints. It's also powerful because it contains more microbes than a person has cells in their body.
In the future, it will increasingly be used not only for diagnosis and for treatment, but for prevention, too. We are heading towards an era of medicine that would have been regarded as the stuff of science fiction 40 years ago, El-Omar says.
It will be a time when an analysis of a poo sample will not only be able to predict a person's risk of diseases, from diabetes to depression, but will be able to help them to restore the health of their biome and minimise those risks.
El-Omar, director of Australia's first Microbiome Research Centre, which is preparing to open its doors in early 2019, describes the biome as a new frontier in medicine.

Photo: Shutterstock
People who suffer from intractable diarrhoea are already swallowing bits of healthy human excrement from donors. Fortunately, it is freeze-dried and packed into capsules, jokingly known as “crapsules”. Their diarrhoea is caused by the bug Clostridium difficile, known as C. diff, and can result in life-threatening inflammation of the colon.
It usually affects older adults and can spread, like a bushfire, through hospitals and residential homes.
In recurrent cases, the first line of treatment in major hospitals around the world is now a faecal microbiota transplant, FMT, during which faeces from a healthy donor is pumped into the small intestine or colon of the patient. This overwhelms the C. diff and, in most cases, people are cured.
We each inherit fixed genes that carry our inherited predisposition to disease. Some of these diseases never eventuate but sometimes something in the environment triggers the relevant genes and one of these diseases appears.
“Almost everything we do is dictated by the interaction between us and our genes and this interface,” says El-Omar. “I can't think of anything else that would have such a profound effect on the way we develop and are able to fend off insults and injuries as we grow older than the microbiome in combination with our genetics.”
He says investigating the biome pulls together every medical speciality, every discipline of science and every discipline of research.
While a few diagnostic tools and treatments related to the gut biome are already in use, they are just scratching the surface. The potential is enormous and could generate a massive industry with many commercial opportunities.
Although research about the gut biome “is pouring out” around the world, El-Omar says the hype is ahead of the science.
Trillions of tiny organisms live in the warm, moist, nutrient-rich environment of the human colon.
This is a busy community with bacteria, viruses, fungi and other microbes intermingling, producing byproducts and interacting with their host.
It's called the gut biome and is the subject of intense international scientific investigation.
Some say the gut biome is the new frontier in medicine and most agree it can exert significant influence on human health.
One way it does this is to cross into the bloodstream. Microscopic organisms or their byproducts traverse the colon wall and once launched into the bloodstream can travel anywhere to do good or cause harm.
Understanding it is an international task for an army of researchers.
And that's just the gut biome. Little microbe communities exist in every nook and cranny of the human body, from the ear canal to the urinary tract, the mouth to the vagina. But the one in the colon is probably the biggest and is thought to exert the greatest influence on our health.
While enthusiasts have been working on the biome since the 1990s, researchers began to organise formally this century. In 2007, the US launched its Human Microbiome Project. In 2008 it began analysing a handful of samples from 300 people.
The aim was to characterise the complexity of the microbe communities at various body sites. Its report in 2013 generated global interest. Now it is in its next phase, creating experimental test beds to evaluate new models, methods and analyses on the interactions of host and microbiome.
There have been equivalent programs in Europe and Asia, and many countries are in the process of creating their own research centres.
Australia's Microbiome Research Centre is due to open early next year. It was allocated an initial $4 million by the federal government in 2017, with the expectation that it will become a world leader in the field.
Earlier this year, it was given a funding boost, with the NSW government committing $1.5 million and South East Sydney Local Health District $1 million to the completion of the centre in southern Sydney.
Based at Sydney's St George and Sutherland Clinical School, UNSW, it plans to draw on the expertise of a wide range of medical specialists, scientists and students.
Just weeks ago, entrepreneur Naveen Jain told The Wall Street Journal's Future of Everything Festival, that his biotech business will make illness “optional”. Jain's lab studies the bacteria in a person's gut using blood, urine, stool and saliva samples, and uses artificial intelligence to make recommendations about what foods will help stave off diseases such as Parkinson's or Alzheimer's.
It's a pitch that appeals, despite a lack of science to back up the claims, and Jain says the company has tens of thousands of customers.
Whatever the evidence, curiosity about the power of the gut biome is booming and can be seen in the healthy online trade in biome kits and tests and by the proliferation of probiotics on chemist shelves. Bookstores around the world are being filled with self-help books on how to build a beautiful biome, but we are nowhere near getting it right.
Last year, a study showed “ridiculously healthy” elderly people have the same gut biomes as healthy 30-year-olds. It involved 1000 Chinese individuals aged three to 100 but its authors couldn't tell which came first. Had the active healthy 90-year-olds eaten well and remained active all their lives or was their healthy state predicated by the good microbes in their gut?
Every few days now, more studies emerge, linking the biome to more conditions, from arthritis to autism, cancer to chronic fatigue, and from MS to mental health. The range is immense. While one study has shown how chronic fatigue syndrome is linked to the biome, another suggested gut bacteria drive the formation of thin walled blood vessels in the brain that can cause strokes and seizures.
"Unlike genetics, the microbiome is something we can change and manipulate. We need to understand gut bacteria and how imbalances occur in a much deeper way if we are to make further advances through clinical trials."
As editor-in-chief of Gut, a leading international journal in gastroenterology, El-Omar is across most new research.
“Perhaps the most exciting of all is the link with mental health. We always thought there was a gut-brain axis but couldn't quite figure out why. Now the mechanisms are dissected out beautifully and being published in the top scientific journals,” he says.
We all know about gut instinct, butterflies in the stomach and how terror turns bowels to water, but now there's emerging evidence of the gut biome being involved in disorders such as depression and anxiety.
When El-Omar first qualified as a gastroenterologist more than 20 years ago, the bowel and its inhabitants were viewed differently and attracted much less interest.
“We referred to them as microflora but that was wrong because these organisms are not plants. That finally got weeded out of the lexicon and now all talk is about the microbiome and interest in it has grown exponentially over the past decade, particularly over the last three or four years.”
So why the sudden rise in interest?
For a long time, researchers had been dependent on the slow, labour-intensive process of culturing microbes. As 80 to 85 per cent of the microbes in the gut can't be cultured, it was equivalent to working with the tip of an iceberg and missing much of the biodiversity below.
Then came fast, cheap gene sequencing and suddenly, instead of culturing bugs, their genomes could be sequenced quickly and their blueprints laid bare. This mini-industrial revolution meant that more species than thought possible were found and, as their roles were disclosed, so the science of the gastrointestinal tract was transformed.
Scientists around the world sat up and the old notion that organisms in the bowel were contaminants that should be cleaned out, was cleaned out itself. It was replaced with the belief that many of these organisms were doing excellent work.
And so, over the past decade, the colon was gradually reconceptualised. No longer was it seen simply as a conduit for waste with a few other functions. It became the site of the gut biome, a major engine for health.
“Unlike genetics, the microbiome is something we can change and manipulate. We need to understand gut bacteria and how imbalances occur in a much deeper way if we are to make further advances through clinical trials,” El-Omar says.
Many years ago, when the work of Sydney gastroenterologist Professor Tom Borody was first reported in the media, readers were aghast. He was the first person to perform faecal transplants in Australia and his colleagues did not approve. Most had never heard of such a thing and couldn't believe it was happening.
There is documented evidence of such transplants being used as therapy in China in the fourth century and they were known to be in use in the US as early as the 1950s.
Borody, now an adjunct professor at UTS in Sydney, conducted his first transplant in 1988 because he had “a patient in need”. He'd come across a paper, published in 1958, in which an antibiotic-associated inflammatory condition had responded to restoration of bowel flora. It was by a doctor who, he says, “with great vision, did four enema faecal transplants in Colorado”.
Borody decided to try it and it worked. Despite opposition, he persisted and the striking results he achieved with treating C. diff, and that have now been replicated by others, here and abroad, helped to drive this field of medicine forwards.
Borody, who since founded the Centre for Digestive Diseases in Sydney's inner west, was way ahead of his time. He would tell people that “poo is a zoo” full of living animals and is itself a living organ. His clinic has performed more than 14,000 faecal transplants and about eight years ago he started the first “brown bank” in Australia to store healthy samples of faeces that are rich in good bacteria.
He has teams of selected donors who, for a fee, drop their stools off at his centre.
He also has a research department that documents cases and conducts clinical trials to try to advance the science of the gut microbiome. One of his goals is to ensure that before he dies, all the children facing losing their bowels because of ulcerative colitis are cured, keep their bowels and live a healthy life.
Now, together with other Australian researchers, he has produced evidence that a faecal transplant can also help in some cases of ulcerative colitis. He co-authored an Australian study, published in The Lancet last year, which showed faecal transplant was a promising new therapeutic option for ulcerative colitis.
The authors said future work should focus on precisely defining the optimum treatment intensity and the role of matching the microbial profiles of donor and recipients. And this is the challenge.
While the database on these microbes is growing fast, a vast amount of work remains to be done to identify and classify them all, figure out what each one does, how they interact under different circumstances and what this means for the host.
Such is the international interest in faecal transplantation that there are now about 200 registered trials of varying quality underway on the subject around the world. Some relate to how the biome can affect the outcome of chemotherapy.
Late last year, a melanoma study published in the prestigious journal Science, showed how the DNA signature of a microbiome can predict whether a patient would respond to immunotherapy.
Next, it showed it was possible to transfer this responsiveness to mice. Those mice that received faecal transplants from the responsive patients did well, while those from resistant patients did poorly.
Another cancer study, published in the British Journal of Surgery, suggested that after surgery for colon cancer, the microbe community that lies adjacent to the site of surgical wound might play an active role in influencing whether the cancer recurs.
While studies like these are at the high end of the research spectrum, there are many at the low end that are reported with equal eagerness. And now, there is so much unbridled enthusiasm in the field, discrimination can be difficult.
Since Harvard professor of public health William Hanage warned four years ago that the microbiome risks being “drowned in a tsunami of its own hype”, waves of fanciful claims have continued to splash into the media. To describe the overselling of the microbiome, University of California microbiologist Professor Jonathan Eisen coined the term “microbiomania”.
He runs a blog called The Tree of Life that hands out awards to those who oversell it and he has had no shortage of candidates, including the uncritical reporting on Lauren Petersen's research on cyclists.

Emad El-Omar, Professor of Medicine at the St George and Sutherland Clinical School, UNSW Sydney, and the Director of the Microbiome Research Centre. Photo: Supplied
While El-Omar, a gastroenterologist, clinician scientist and professor of medicine at UNSW, says he is excited by the science, he's extremely cautious about introducing interventions that are not rigorously tested and proven to work.
“To a number of companies, you can already send in a stool sample and get an analysis but their analysis is based on theory alone. We haven't done the studies yet.”
Would he take off-the-shelf probiotics?
“I would be the first to take them if I could find a formula that had been proved clinically, in adequately powered studies, to show it makes a difference. But these are being sold as food supplements, like vitamins.”
People are talking about the possibility of going biome shopping, perhaps for one that might eliminate diabetes, make them thinner or more energetic. Would he have a faecal transplant?
“While theoretically feasible, it is jumping the gun because no one knows what is lurking in an apparently attractive biome.
“Obvious pathogens such as HIV, hepatitis and salmonella can be excluded, but how does anyone know there aren't other nasties or that the microbe mix from that particular donor will be good for them?
“A personalised scientific approach is necessary to determine what the recipient needs and whether the donor has it.”
“Ultimately, the best biome you can have may well be your own,” says Professor Mark Morrison, a microbiologist at The University of Queensland Diamantina Institute.
While your biome begins to form at birth and consolidates over the first 1000 days of your life, it always remains somewhat in flux.
It sounds bizarre, but it is not beyond imagination that one day people may store biome samples for when they are unwell, just as people now store their own blood in case they need a transfusion. There will also be opportunities partially to rebuild a biome after a procedure such as colonoscopy. The “prep” taken to purge the bowel in advance wipes out much of the gut biome.
If we knew what the ultimate biome looked like, one could be inserted once the colonoscopy was over. But we don't.
Morrison spends his days eavesdropping on the crosstalk in the biome, investigating how the inhabitants interact with one another, their environment and their host to maintain homeostasis, a healthy equilibrium.
Unusually, the team he leads works in a biomedical research unit and when a gastroenterologist passes one of them a sample of faeces or mucus from the lining of a patient's bowel, they examine it for insights about the patient's symptoms.
The decades Morrison spent culturing organisms enable him to make a more meaningful interpretation of genetic sequencing.
“Just a small sample allows you to produce enough DNA sequence information to give you a kind of wiring diagram, of the functional aspects associated with the microbes present in it.”
The point is not only to diagnose the problem and devise therapy for it, but to try to detect disease processes early enough to prevent their development.
“If a patient has a family history of Crohn's disease [inflammation of the gastrointestinal tract], their microbiome may provide the opportunity to identify the changes that are starting to take place before the actual disease starts. The hope is that something can be done to thwart or prevent those changes progressing.”
His team is also working on identifying products from microbes that can be absorbed across the gut, enter into the bloodstream and potentially influence the body's chemistry and immune systems.
“Many of these factors and the genes encoding them are still undefined, and what we might call microbial dark matter,” he says.
In animal models, and some clinical studies of type 2 diabetes, obesity and other metabolic diseases, perturbations in the gut microbiome have been linked with these conditions, and there is real promise that introducing specific micro-organisms into the digestive tract may partially reverse the process.
But it is very early days and he is wary of calling the microbiome the cause, the consequence or the cure of this and other metabolic conditions.
“It's premature. The microbiome is like a dark continent, it's like going to Africa for the first time. There are a lot of unknowns and while we are making exciting findings and must keep going, we also need to be balanced and pragmatic, working closely with our clinical colleagues.”
On treatment, Morrison says one aim is to move away from faecal transplants and create a smart generation of probiotics, personalised for an individual patient's condition. After determining exactly which microbes the patient needs, these can be placed in a capsule.
On prevention, he says we need to know what a healthy microbiome looks like so an unhealthy one can be identified. This will help in deciding what lifestyle and diet changes need to be made to drive a disturbed microbiome back into balance and so improve the patient's resilience and protect them against the triggering of an unwanted condition.
A good example, he says, is the FODMAP diet developed by Monash University researchers to provide relief from irritable bowel syndrome, IBS.
FODMAPS are sugars and polyols (low-digestible carbohydrates that taste like sugar) that are not absorbed in the small intestine. When they reach the colon, and are digested by the gut microbiota, this can trigger symptoms in people with IBS. Reduce them and the symptoms are reduced in many but not all IBS patients.
“We are still trying to figure out what causes this syndrome and exactly how this diet works,” he says.
While Morrison is as enthusiastic about the gut biome as anyone else, he's cautious. The long-term effects of manipulating it are not known and there are ethical issues to be considered.
We have reached the dark continent, he says, but we are only on its coastal fringes. There is much uncharted territory still to cover.
Jill Margo is an Adjunct Associate Professor at UNSW.
This article was originally published on the . Read the .